Abstract
The central regulator of erythropoeitic rate is erythropoietin (Epo). Epo action is augmented by factors that act on early erythroid progenitors upstream of erythroid terminal differentiation: glucocorticoids, Stem Cell Factor and BMP4. Of these, only Epo and glucocorticoids are useful agents clinically, leaving a gap when they are ineffective or contraindicated. The molecular identities of early erythroid progenitors are not well understood, posing an obstacle to the discovery of novel erythropoietic agents. To address this gap, we used single-cell RNA-seq (scRNA-seq) technology to delineate a continuous erythroid trajectory in the mouse, beginning with multi-potential progenitors (MPPs) and ending with the onset of erythroid terminal differentiation (described in Tusi, Wolock et al.). Based on gene expression analysis, we predicted two novel developmental stages within the erythroid trajectory, that we termed Early Erythroid Progenitors (EEP) and Committed Erythroid Progenitors (CEP). We devised a flow cytometric strategy that enriches for these novel progenitor stages, and found that they correspond to cells with BFU-e and CFU-e activity, respectively.
Our scRNA-seq work predicted cell surface molecules expressed by EEPs and CEPs, including receptors with known endogenous ligands or drug agonists or antagonists, but no previously documented role in erythropoiesis. The first three such receptors that we tested, Mst1r, Ryk and IL-17RA, all modified adult and/or fetal liver BFU-e and CFU-e colony formation in vitro . In the case of IL-17RA, its IL-17a ligand cooperated synergistically with Epo to expand the number of adult bone marrow CFU-e in vitro, while having no effect on fetal liver CFU-e. Specifically, at the modestly elevated Epo concentration of 0.05 U/ml, addition of IL-17a (10 ng/ml) resulted in a 2.5 fold increase in CFU-e colonies (p<0.001); at levels of Epo that elicit its maximal effect (2 U/ml), addition of IL-17a increased the number of CFU-e colonies by an additional 44% (p=0.002). A dose response analysis showed that EC50 for IL-17a's synergistic action with Epo was 2 ng/ml (60 pM). Furthermore, addition of IL-17a boosted the formation of human bone marrow CFU-e but not BFU-e in vitro .
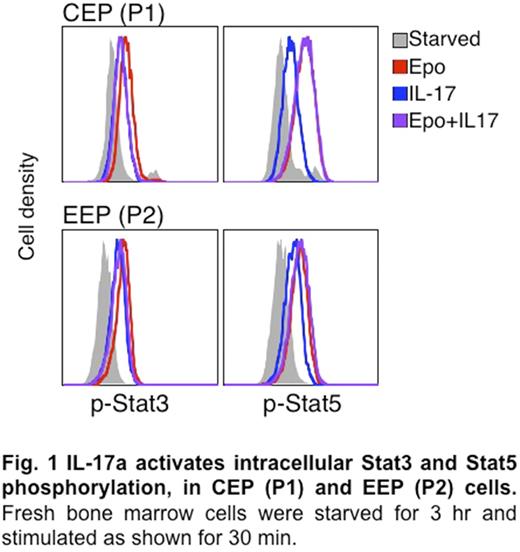
IL-17a had no effect on CFU-e formation in bone marrow derived from IL-17RA-/- mouse, confirming the specificity of this interaction. In work that is ongoing, we found that IL-17a activated intracellular Stat3 and Stat5 signalings in early erythroid progenitors. Taken together, these findings suggest that IL-17a is a novel erythropoietic stimulator, synergizing with Epo to accelerate erythropoietic rate.
Klein: OneCell Bio: Other: Equity Ownership and Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal